Understanding Menopause Symptom Management
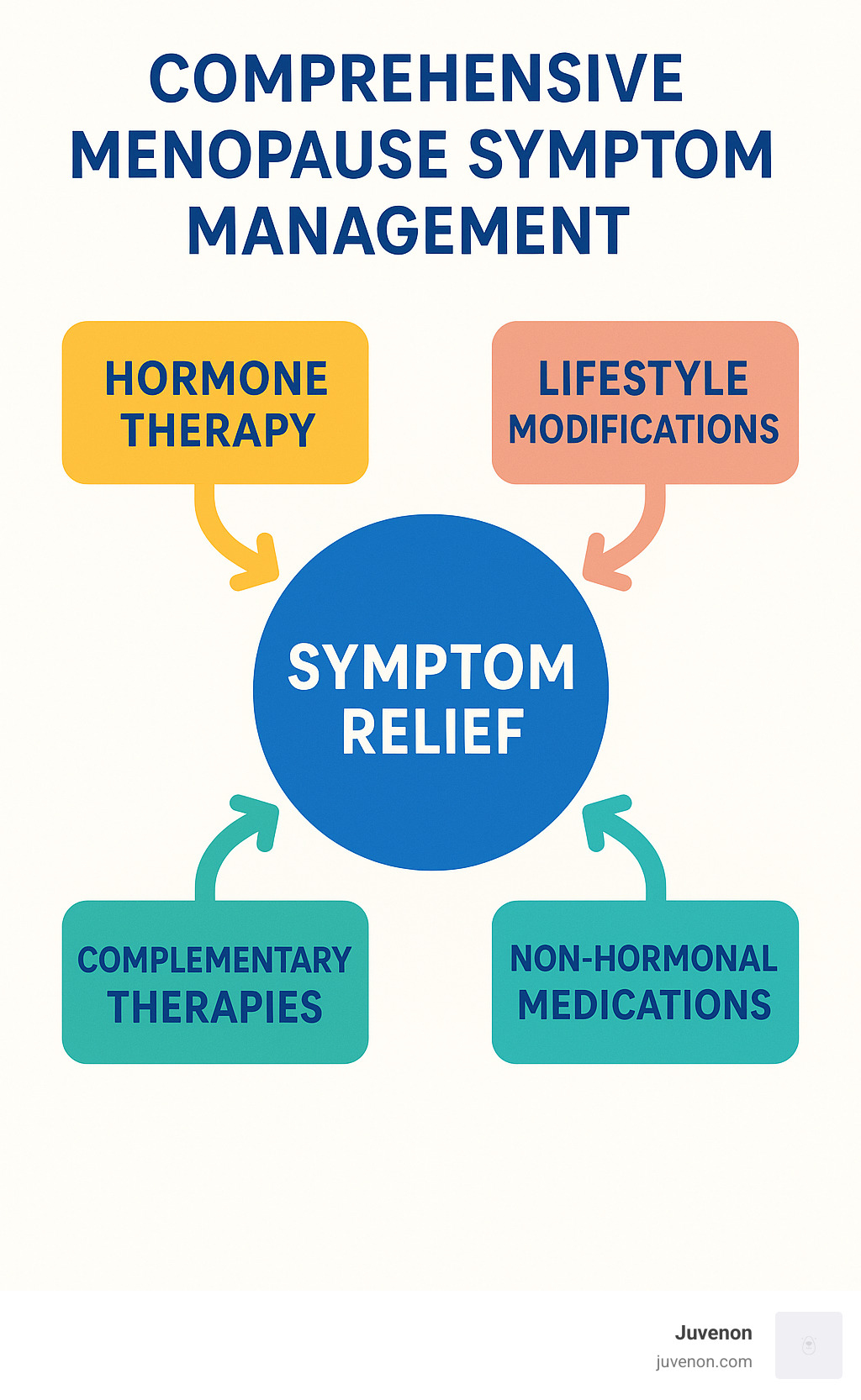
Menopause system management refers to the comprehensive approach to addressing the physical, emotional, and long-term health impacts of menopause through medical treatments, lifestyle changes, and complementary therapies.
For quick reference, effective menopause system management includes:
- Hormone therapy - when appropriate based on individual risk factors
- Non-hormonal medications - including SSRIs, gabapentin, and fezolinetant
- Lifestyle modifications - diet, exercise, stress reduction
- Complementary therapies - acupuncture, mindfulness, CBT
- Regular health screenings - bone density, cardiovascular, cancer screenings
Menopause is not a medical problem but a natural life transition that typically occurs around age 51. However, the symptoms that accompany this change can significantly impact quality of life for many women. From hot flashes and night sweats to sleep disturbances and mood changes, the menopausal transition affects each woman differently.
About 75% of women experience hot flashes during menopause, with many continuing to face them for more than seven years post-menopause. This isn't just about discomfort - these symptoms can disrupt sleep, work performance, and overall wellbeing.
The good news? We now understand that menopause symptoms can be effectively managed through a personalized, systematic approach that addresses the whole person.
I'm Michelle M. Henson, a copywriting leader with extensive experience researching and developing content related to menopause system management, having helped countless women steer this transition through evidence-based information during my tenure at Juvenon and as a health content specialist.
Menopause 101: Causes, Stages & Diagnosis
Think of menopause as a gradual sunset rather than flipping off a light switch. Your body doesn't suddenly stop producing hormones overnight—instead, your ovaries slowly decrease their production of estrogen and progesterone over time. This natural ovarian aging process is simply part of your life's journey.
Most women reach natural menopause around age 51, though anywhere from your mid-40s to mid-50s falls within the normal range. If menopause arrives before age 40, doctors consider it premature menopause, which can happen spontaneously or result from medical treatments like chemotherapy, radiation, or surgery to remove the ovaries.
How do you know when you've officially reached menopause? The "12-month rule" is the gold standard—when you've gone a full year without a menstrual period, you can officially say you've reached menopause.
Stages & Hormone Shifts
Menopause system management begins with understanding that this transition unfolds in distinct chapters:
-
Perimenopause - The "lead-up" years that typically begin in your 40s. This stage can last 8-10 years, with symptoms becoming more noticeable in the final 1-2 years as hormone levels fluctuate dramatically.
-
Menopause - The milestone marking 12 consecutive months without a period.
-
Postmenopause - All the years that follow for the rest of your life.
Healthcare providers often use the STRAW+10 (Stages of Reproductive Aging Workshop) criteria to map where you are in this journey and determine appropriate care strategies.
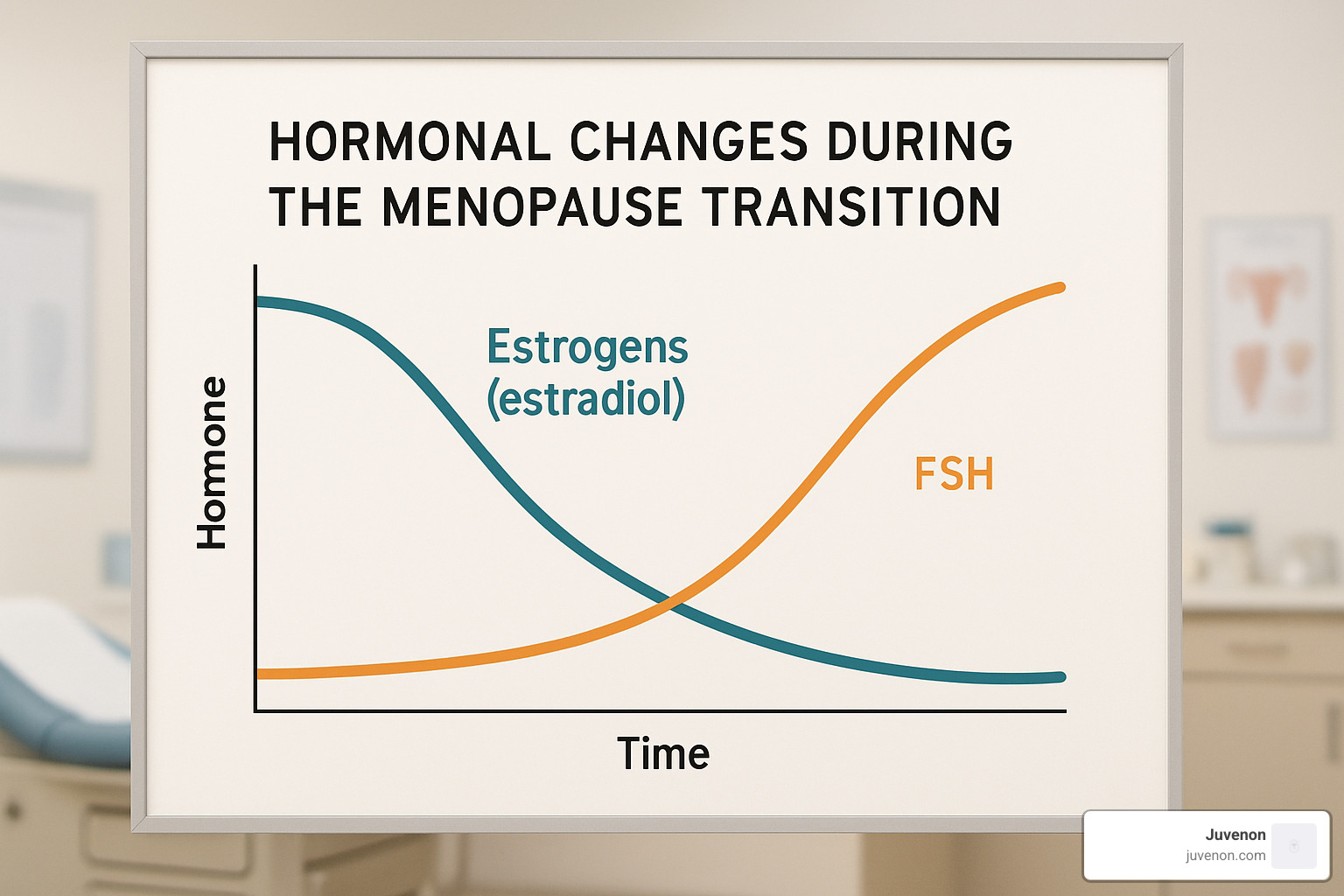
During perimenopause, your remaining ovarian follicles become less responsive to follicle-stimulating hormone (FSH). Think of it as your ovaries needing a louder "wake-up call"—so your body increases FSH levels trying to stimulate them. Luteinizing hormone (LH) also rises, while estradiol (your main form of estrogen) swings up and down like a roller coaster before eventually declining. Another hormone called anti-Müllerian hormone (AMH) decreases as your follicle count diminishes, providing doctors with a useful marker of your ovarian reserve.
Confirming the Transition
While the 12-month rule definitively confirms menopause, your healthcare provider might use several approaches to assess where you are in the transition:
Clinical history is often the most practical tool. Your doctor will track your menstrual patterns and symptoms to create a timeline of your transition.
Laboratory markers can provide supporting evidence—FSH levels above 30 mIU/mL suggest menopause, though a single measurement isn't conclusive because these levels can fluctuate wildly during perimenopause.
AMH testing offers another perspective, as low levels indicate your ovarian reserve is diminishing.
Your doctor will also consider differential diagnoses, ruling out other causes of menstrual changes such as thyroid disorders, liftd prolactin levels, or pregnancy.
It's worth noting that hormone tests aren't always necessary or definitive. For most women, the pattern of symptoms and menstrual changes tells your healthcare provider everything they need to guide appropriate menopause system management. Your lived experience—the hot flashes, sleep disruptions, and menstrual changes—often speaks louder than any blood test.
Menopause System Management: Goals, Planning & Monitoring
Navigating menopause doesn't have to feel like charting unknown waters. Think of menopause system management as your personalized roadmap—one that considers your unique symptoms, health history, and what matters most to you.
At its heart, effective menopause system management focuses on four essential goals:
- Taming those bothersome symptoms that might be disrupting your daily life
- Protecting your long-term health from risks associated with estrogen decline
- Maintaining (or even improving!) your quality of life
- Creating a care approach that feels right for you as an individual
Have you heard of the "timing hypothesis"? Research suggests that starting hormone therapy within 10 years of menopause or before age 60 offers the sweet spot—maximizing benefits while keeping risks to a minimum. This highlights why being proactive rather than reactive can make all the difference in your menopause journey.

Core Principles of Menopause System Management
When it comes to managing your menopause experience effectively, several principles stand out as particularly important:
Your voice matters most in treatment decisions. After all, it's your body and your experience. The best plans reflect your personal goals, preferences, and values—not just clinical guidelines.
Weighing benefits against risks is crucial for each potential treatment. What works wonderfully for your friend might not be right for you, depending on your health history and risk factors.
Starting with the lowest effective dose of any medication helps minimize potential side effects while still providing relief. You can always adjust upward if needed.
Regular check-ins with your healthcare provider keep your plan on track. Typically, you'll want a follow-up about three months after starting any new treatment, then annually to reassess how things are working.
The North American Menopause Society emphasizes the importance of maintaining an ongoing relationship with healthcare providers throughout this transition and beyond. Think of these appointments not as a chore but as a partnership that helps you thrive during this new chapter.
Creating Your Personal Plan
Building your personalized menopause system management strategy starts with becoming your own best health detective:
Start by tracking your symptoms in a simple diary. Note what you're experiencing, how often, how severe it feels, and how it's affecting your daily life. This information is gold when discussing options with your healthcare provider.
Next, work with your provider to assess your personal health risks. Tools like QRISK (for cardiovascular disease) and FRAX (for fracture risk) can help paint a clearer picture of what preventive measures might benefit you most.
Take time to identify your priorities. Which symptoms are making the biggest impact on your quality of life? For some women, hot flashes disrupt sleep and work. For others, mood changes or vaginal dryness might be more concerning.
Finally, ensure good communication between all your healthcare providers. Your primary doctor, gynecologist, and any specialists should be on the same page about your menopause management plan.
Your needs will likely evolve as you move through the menopause transition. What works during early perimenopause might need adjustment as you enter postmenopause. The beauty of a well-designed menopause system management plan is that it grows and changes with you, supporting your health and well-being at every stage.
Think of this as a shared decision-making journey where you and your healthcare team work together to find the right balance of treatments, lifestyle changes, and monitoring that helps you feel your best. After all, menopause isn't just something to "get through"—with the right approach, it can be a gateway to a healthy, vibrant next chapter.
Evidence-Based Treatments: Hormonal & Non-Hormonal Options
When it comes to menopause system management, there's no magic bullet that works for everyone. Each woman's experience is unique, which is why we have various treatment options to choose from. Let's explore what science tells us works best.
Hormone Replacement Therapy Essentials
Hormone replacement therapy (HRT) remains the gold standard for tackling those pesky hot flashes and night sweats that can make life miserable. It's like giving your body back what it's missing.
"I was skeptical at first," many women tell me, "but hormone therapy gave me my life back."
HRT comes in several forms to suit your needs:
Systemic estrogen therapy delivers relief through pills, patches, gels, or sprays that address multiple symptoms at once. If you still have your uterus, you'll need estrogen-progestogen therapy (EPT) because the progestogen protects your endometrium from cancer risk. Had a hysterectomy? Then estrogen-only therapy (ET) might be your ticket to relief.
For women concerned about systemic effects, low-dose vaginal estrogen in creams, tablets, or rings can target local symptoms with minimal absorption into your bloodstream.
The delivery method matters too. Transdermal (skin) patches bypass your liver, reducing blood clot risks and potentially offering heart benefits. This route is particularly wise if you have migraine with aura, high triglycerides, or liver concerns.
The benefits can be remarkable—75-90% fewer hot flashes, better sleep, relief from vaginal dryness, and protection against bone loss (increasing spine bone density by 10.6% and hip density by 5.5% over two years). Some research even suggests a possible reduction in heart disease when started early.
But what about the risks? Yes, there's a slight increase in breast cancer risk with long-term use of combined therapy, and oral estrogen (but not patches) can increase blood clot risk. The key is timing—starting within 10 years of menopause maximizes benefits while minimizing risks.
Remember to schedule regular mammograms if you're on HRT, and check in with your healthcare provider annually to reassess your treatment plan.
Non-Hormonal Pharmacologic Arsenal
Not everyone can or wants to use hormones, and that's perfectly okay. Science has given us several effective alternatives:
SSRIs and SNRIs like paroxetine (the only FDA-approved non-hormonal treatment for hot flashes), venlafaxine, and escitalopram can reduce hot flashes by 40-60%. They're particularly helpful for women who also experience mood changes.
A breakthrough medication called fezolinetant (Veozah), a neurokinin-3 receptor antagonist, specifically targets the brain circuits responsible for hot flashes. Many women find it gives relief without hormonal effects.
Gabapentin and pregabalin, originally developed for seizures, can be your allies against night sweats while improving sleep quality. Clonidine, typically used for high blood pressure, offers modest hot flash relief for some women.
For those struggling with painful intercourse, ospemifene, a SERM, specifically addresses this symptom. And if bone health is your concern, bisphosphonates and denosumab prevent bone loss and reduce fracture risk.
Your healthcare provider can help match these options to your specific symptoms and health history. As with any medication, each has its own benefit-risk profile worth discussing.

Managing Hot Flashes & Night Sweats
Hot flashes can strike without warning, leaving you drenched and uncomfortable. A smart approach combines lifestyle tweaks with medical options.
First, become a detective and identify your personal triggers. Spicy foods, alcohol, caffeine, hot drinks, and warm environments are common culprits. Dressing in layers lets you adjust quickly when that internal furnace kicks on.
Keep your environment cool—fans, lower thermostat settings, and ice water can be lifesavers. Many women find that slow, deep breathing (paced breathing) can actually reduce both the frequency and intensity of hot flashes.
When night sweats disrupt your sleep, try moisture-wicking pajamas and sheets, and keep your bedroom cool (around 65°F/18°C). Good sleep isn't just about comfort—it's essential for cellular repair, brain function, and metabolic health.
For more strategies on managing sleep disruptions naturally, check out our article on Managing Menopause Sleep Disruptions Without Medication.
Genitourinary & Sexual Health
The changes "down there" during menopause can be distressing but are treatable. As estrogen declines, many women experience vaginal dryness, painful sex, urinary urgency, frequent UTIs, and decreased desire.
Vaginal moisturizers work like skin moisturizers, restoring comfort and pH balance. Look for those containing hyaluronic acid for longer-lasting relief. Lubricants (water- or silicone-based) can make intimate moments comfortable again.
Local estrogen therapy delivers tiny amounts of estrogen directly to vaginal tissues through creams, tablets, or rings, often with minimal systemic absorption. Many women find this approach offers relief without concerns about systemic hormone therapy.
Don't overlook the power of pelvic floor physical therapy, which can strengthen muscles and improve urinary symptoms. And for libido concerns, some healthcare providers may suggest testosterone gel off-label, though it's not yet FDA-approved for women.
A simple technique for urinary symptoms: try double-voiding—urinate, wait a moment, then try again to ensure your bladder empties completely.
Addressing these intimate concerns is an essential part of menopause system management. You deserve to feel comfortable in your body at every stage of life.
For more information about hormone balance through nutrition, explore our article on Top 10 Hormone Balancing Foods and learn how what you eat can support your body's natural processes.
Lifestyle Upgrades & Complementary Therapies
When it comes to taming menopause symptoms, medications aren't your only allies. The foundation of effective menopause system management often starts with simple changes to your daily habits and routines that can make a world of difference.
Daily Habits That Ease Symptoms
Think of your lifestyle choices as the base of your menopause wellness pyramid. Small, consistent changes can yield impressive results in how you feel day to day.
Embracing a Mediterranean-style diet rich in colorful fruits, leafy vegetables, whole grains, and healthy fats isn't just good for your heart—it may actually reduce how often those pesky hot flashes pay you a visit. Your bones will thank you too if you aim for about 1,200 mg of calcium and 800 IU of vitamin D daily, especially as menopause increases your risk of bone loss.
Moving your body regularly works wonders during this transition. Aim for 150 minutes of moderate activity each week (that's just 30 minutes, five days a week!) plus a couple of strength-training sessions to support your muscles, mood, and metabolism. Many women find that even modest weight loss—just 5-10% of body weight—can actually shorten how long hot flashes stick around.
Sleep hygiene becomes especially important when night sweats threaten your rest. Try keeping your bedroom cool (around 65°F is ideal), sticking to consistent bedtimes, and putting away those tempting screens at least an hour before bed. If insomnia persists, cognitive behavioral therapy for insomnia (CBTi) has shown impressive results specifically for menopausal women.
Learning to manage stress isn't just good for your sanity—it can directly impact your symptoms. Whether it's through mindfulness meditation, gentle yoga, or simply taking five minutes for deep breathing throughout your day, finding your calm can reduce stress-triggered hot flashes.
And speaking of triggers, pay attention to what sets off your personal hot flash alarms. For many women, cutting back on caffeine, alcohol, and spicy foods can make a noticeable difference in symptom frequency.

At Juvenon, we understand that cellular energy often takes a hit during menopause, contributing to that all-too-common fatigue. Our supplements are specifically formulated to support mitochondrial function—your cells' power plants—to help you maintain energy and vitality during this transition.
Complementary & Alternative Options
Many women find relief through approaches that complement conventional medicine. These can be particularly helpful for those who can't or prefer not to use hormone therapy.
Phytoestrogens—plant compounds with mild estrogen-like effects—can be found in foods like soy, flaxseeds, and chickpeas. While not as powerful as medical hormone therapy, some women report symptom improvement when incorporating these foods regularly. If you're considering soy isoflavone supplements, keep it under 25g daily and check with your doctor first, especially if you have a history of hormone-sensitive cancers.
Herbal remedies have been used for centuries to ease menopause symptoms. Black cohosh is among the most studied, with some women finding it helpful for hot flashes (though clinical trials show mixed results). Red clover and evening primrose oil have their devotees as well, though scientific evidence remains limited.
Acupuncture deserves consideration too—several studies suggest it may reduce hot flash frequency and improve sleep quality. The tiny needles seem to help restore balance in the body's energy systems, potentially modulating the hormonal fluctuations that trigger symptoms.
Mind-body practices like yoga, tai chi, and qigong offer the double benefit of gentle movement paired with stress reduction—a powerful combination for symptom management. The mindful breathing incorporated in these practices may help reduce hot flash intensity when they do occur.

A word of caution about complementary approaches: "natural" doesn't automatically mean safe. Choose high-quality products from reputable sources, and always keep your healthcare provider in the loop about what supplements you're taking. Many can interact with medications or aren't appropriate for certain health conditions.
For more guidance on foods that can help balance your hormones naturally during menopause, check out our article on Top 10 Hormone Balancing Foods, where we explore delicious options that support your body during this transition.
Long-Term Health Risks & Prevention Strategies
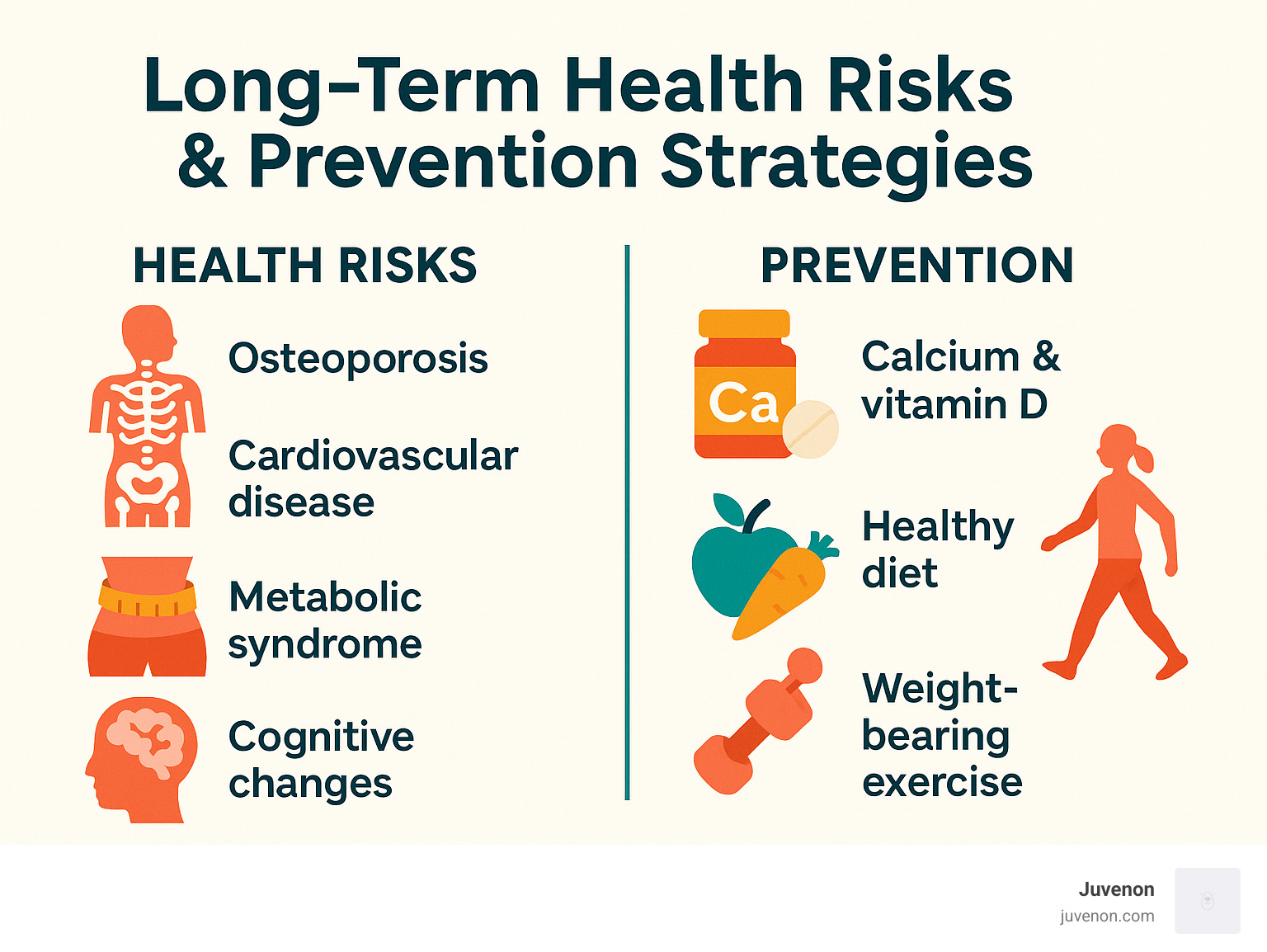
Menopause system management isn't just about tackling those immediate hot flashes or mood swings—it's about protecting your future self too. The estrogen decline that comes with menopause creates some serious health challenges we need to address.
Did you know that women lose about 25% of their bone mass between menopause and age 60? That's a lot! This rapid bone loss opens the door to osteoporosis and increased fracture risk. In the U.S. alone, over 250,000 hip fractures happen each year, and sadly, many lead to loss of independence or even worse outcomes.
But bone health is just one piece of the puzzle. After menopause, your risk increases for: - Cardiovascular disease (heart attacks and strokes) - Metabolic syndrome (a cluster of conditions that raise your heart disease risk) - Cognitive changes (those frustrating "brain fog" moments) - Urogenital atrophy (those uncomfortable vaginal and urinary symptoms)
Bone & Joint Protection
Think of your bones as your body's framework—they need extra care during this transition. Here's how to keep them strong:
Weight-bearing exercise does wonders for maintaining bone density. This doesn't mean you need to become a gym rat! Walking, dancing, gardening, or even climbing stairs all count. The key is to choose activities where your bones and muscles work against gravity.
Calcium and vitamin D work as a dynamic duo for bone health. Your body needs calcium to build bone, and vitamin D helps absorb that calcium. Aim for 1,200 mg of calcium daily through diet and supplements if needed. For vitamin D, 800-1,000 IU daily is typically recommended.
Regular bone density screening is crucial. A DEXA scan is recommended for all women 65 and older, but if you have risk factors like family history or early menopause, you might need screening sooner. Don't skip this important test!
When lifestyle measures aren't enough, medication can help. Bisphosphonates like alendronate or medications like denosumab can significantly reduce your fracture risk. Scientific research on osteoporosis drugs continues to evolve, giving us better options each year.
Timing matters too! Starting hormone therapy within three years of menopause provides the best bone protection, reducing hip fracture risk by up to 35%. That's pretty impressive protection for your skeleton.
Cardiometabolic Vigilance
Here's something that might surprise you: after menopause, a woman's risk of heart disease approaches that of men. The protective effect of estrogen fades, making heart health a top priority.
Regular screening becomes your first line of defense. Get your blood pressure checked every 1-2 years starting at age 40, and have your cholesterol levels tested every 5 years. These simple tests can catch problems early when they're easier to address.
Physical activity remains one of your best heart protectors. Aim for at least 150 minutes of moderate-intensity exercise weekly—that's just 30 minutes, five days a week. Find activities you enjoy, whether it's swimming, cycling, or dancing around your living room!
Following a heart-healthy diet like the DASH or Mediterranean approach provides your body with the nutrients it needs. These eating patterns emphasize fruits, vegetables, whole grains, lean proteins, and healthy fats while limiting processed foods and excess sodium.
If you smoke, quitting now gives your heart immediate benefits. Within just one year of quitting, your heart disease risk drops dramatically.
Maintaining a healthy weight helps control blood pressure, cholesterol, and diabetes risk—all factors that affect your heart. Even modest weight loss can make a significant difference in your heart health.
Interestingly, early intervention with hormone therapy (within 10 years of menopause) may offer some cardiovascular protection, though doctors don't prescribe it solely for this purpose. Your healthcare provider can help you weigh the pros and cons based on your personal health history.
At Juvenon, we understand that cellular health forms the foundation of overall wellness during menopause and beyond. Our scientifically formulated supplements support the mitochondria—your cells' energy powerhouses—which may help maintain metabolic health during this transition. Small steps taken today can lead to better health outcomes tomorrow.
Frequently Asked Questions about Menopause System Management
How long should I stay on HRT?
When it comes to hormone therapy, there's no one-size-fits-all answer. Think of HRT as a personalized journey rather than a fixed prescription.
Current medical wisdom suggests using the lowest effective dose for the shortest time needed to manage your symptoms. For most women who start HRT to tame those pesky hot flashes, treatment typically runs for about 2-5 years. That said, if you're still experiencing significant symptoms after this period, longer use might make sense for you.
This is your body and your experience. I always recommend having regular check-ins with your healthcare provider to reassess how things are going. These conversations help balance the relief you're getting against any potential risks that might change over time.
And if you do decide to stop HRT? Consider the "slow and steady" approach. Gradually tapering your dosage rather than stopping cold turkey can help prevent those symptoms from making an unwelcome comeback.
What can I do if I can't use hormones for menopause system management?
Not everyone can—or wants to—use hormone therapy, and that's completely okay! There are plenty of effective alternatives in your menopause system management toolkit.
If you have contraindications like a history of breast cancer, stroke, or blood clots (or simply prefer non-hormonal approaches), you have several good options:
For hot flashes, FDA-approved medications like paroxetine and fezolinetant can provide significant relief. For painful intercourse, ospemifene might be helpful. Your doctor might also suggest other medications "off-label" such as different types of antidepressants, gabapentin, or clonidine.
Beyond medications, lifestyle changes can make a remarkable difference. Adjusting your diet, getting regular exercise, practicing stress reduction techniques, and avoiding personal triggers often provides substantial relief. For genitourinary symptoms, over-the-counter vaginal moisturizers and lubricants can be game-changers.
Many women find cognitive behavioral therapy helpful for managing hot flashes, sleep troubles, and mood changes. And don't overlook complementary approaches like acupuncture, mindfulness practices, and certain carefully selected supplements.
The beauty of non-hormonal approaches is that you can mix and match to create a personalized strategy that works for your unique situation.
When should I seek medical advice for new or worsening symptoms?
While many menopause symptoms can be managed with lifestyle tweaks and over-the-counter products, certain situations deserve prompt medical attention. Trust your instincts—you know your body best.
Abnormal bleeding should always be evaluated, especially heavy bleeding, bleeding after intimacy, or any bleeding once you've been in menopause for a full year. This isn't something to wait on.
If hot flashes become so severe they're significantly disrupting your sleep or daily activities, it's time to talk with your healthcare provider. Similarly, debilitating mood changes—especially if accompanied by thoughts of self-harm—warrant immediate professional support.
New or worsening urinary symptoms might indicate an infection or other urogenital issues that need treatment. And if you're experiencing memory or concentration problems that interfere with your daily life, don't chalk it up to "just menopause" without discussing it with your doctor.
Persistent pain during intimacy, even when using lubricants, is another reason to seek care. This is often very treatable, and you deserve to enjoy this aspect of your life.
Early intervention for these concerns not only prevents complications but can dramatically improve your quality of life. Addressing these issues isn't a luxury—it's an important part of your overall health care during this transition.
At Juvenon, we believe that thriving during menopause is absolutely possible with the right support and information. While our supplements support cellular health during this transition, working with healthcare providers on a comprehensive menopause system management plan ensures you're covering all your bases.
Conclusion
Menopause system management isn't about fighting against nature—it's about embracing this transition with strategies custom just for you. Think of it as partnering with your body rather than battling it. By thoughtfully combining medical treatments with lifestyle changes and preventive care, you can sail through this transition with fewer disruptions while protecting your health for decades to come.
Many women find that postmenopause brings unexpected gifts—freedom from monthly cycles, a deeper appreciation for self-care, and often a renewed sense of purpose. This stage of life doesn't signal the end of vitality but rather invites you into a new chapter filled with possibilities.
Here at Juvenon, we understand the cellular changes that accompany menopause. Our scientifically backed supplements support the foundation of wellness during this transition—your cellular health. Our patented formulas are specifically designed to nurture mitochondrial function, boost cellular energy, and maintain metabolic health—all areas that typically need extra support during menopause.
Whether you're noticing your first hot flash or you've been navigating postmenopause for years, remember—it's never too late to implement an effective menopause system management plan. Start with one small change today. Partner closely with healthcare providers who listen. And perhaps most importantly, view this transition as an opportunity to recommit to your wellbeing.
The journey through menopause is uniquely yours. Some days will feel challenging, others rewarding. But with thoughtful management and support, you can experience this natural life transition with confidence and grace.
For more insights about proactive approaches to menopause and how Juvenon's supplements can support your journey, explore our article on proactive menopause strategies or reach out to our caring customer service team who can answer your questions.
Your best years aren't behind you—they're unfolding right now.






















