
What causes extreme fatigue and shortness of breath can range from common conditions to serious medical issues. If you're experiencing these symptoms, here's a quick overview of the most common causes:
- Heart conditions: Heart failure, coronary artery disease, arrhythmias
- Lung diseases: COPD, asthma, pulmonary fibrosis, pneumonia
- Blood disorders: Anemia, vitamin deficiencies
- Endocrine issues: Hypothyroidism, adrenal insufficiency
- Infections: COVID-19, influenza, mononucleosis
- Autoimmune conditions: ME/CFS, rheumatoid arthritis
- Sleep disorders: Sleep apnea, insomnia
- Mental health: Anxiety, depression, stress
- Lifestyle factors: Deconditioning, poor sleep, nutritional deficiencies
Fatigue is a lingering tiredness that goes beyond normal exhaustion and isn't relieved by rest. When paired with shortness of breath (dyspnea), these symptoms can significantly impact your quality of life. Unlike normal tiredness, which improves after a good night's sleep, extreme fatigue persists and can make even simple daily activities feel overwhelming.
The combination of these symptoms is particularly concerning because they affect your body's core functions - energy production and oxygen delivery. When your cells can't get enough oxygen or can't use it efficiently, both fatigue and breathing difficulties can result.
I'm Michelle M. Henson, a health content expert with over two decades of experience researching and writing about conditions that cause extreme fatigue and shortness of breath, including working with leading physicians to translate complex medical concepts into actionable information for patients. My background as a legal compliance editor has equipped me to evaluate the scientific evidence behind various causes of these debilitating symptoms.

What Causes Extreme Fatigue and Shortness of Breath? (The Big Picture)
Ever wonder why your body sometimes feels like it's running on empty while you struggle to catch your breath? At the heart of extreme fatigue and shortness of breath lies a fundamental issue: your body's oxygen delivery system isn't working as it should.
Think of your body as a well-orchestrated machine. You breathe in oxygen, it travels to your lungs, transfers to your bloodstream, gets pumped by your heart throughout your body, and finally reaches your cells to help produce energy. When any part of this complex pathway breaks down, you feel the effects as both crushing tiredness and difficulty breathing.
Have you noticed feeling unusually winded after climbing a flight of stairs or carrying groceries? This is called exertional dyspnea. While everyone breathes harder during physical activity, becoming disproportionately breathless from mild exertion often signals something's not right underneath the surface.
The numbers tell a sobering story about how common these issues are. About 30 million Americans (that's 11% of us) struggle with chronic lung disease. Heart disease affects roughly 22 million people (8% of Americans). Anemia impacts more than 5.6% of the population, while about 17% of women will develop thyroid disorders by age 60. And in our post-pandemic world, approximately one in four people who contract COVID-19 develop long-lasting symptoms.
Speaking of viral infections, they deserve special attention. After battling COVID-19, mono, or even a severe case of flu, some people never quite bounce back. These post-viral syndromes can leave you dealing with persistent fatigue and breathing difficulties for months, dramatically affecting your quality of life when you should be feeling better.
What Causes Extreme Fatigue and Shortness of Breath in Heart & Lung Diseases
Heart and lung conditions top the list of medical causes for these twin symptoms. These vital organs work together like dance partners to deliver oxygen throughout your body, and when one stumbles, the performance suffers.
Heart Failure doesn't mean your heart stops—it means it can't pump efficiently. Remember the FACES acronym: Fatigue, Activities limited, Chest congestion, Edema (swelling), and Shortness of breath. About 5 million Americans live with heart failure, and without proper treatment, up to half may die within five years.
COPD progressively damages your airways and tiny air sacs (alveoli), making it harder to breathe in oxygen and expel carbon dioxide. Many patients describe the fatigue as completely overwhelming, turning simple tasks into exhausting ordeals. While smoking is the primary culprit and there's no cure except lung transplantation, treatments can help you breathe easier.
During an asthma attack, your airways narrow and fill with mucus, making every breath a struggle. All that extra effort to breathe burns energy, leaving you exhausted. Plus, the chronic inflammation in your lungs can contribute to whole-body fatigue.
Pulmonary Hypertension involves thickening and stiffening of the arteries in your lungs, forcing your heart's right side to work overtime. The result? Often severe fatigue and breathlessness, especially when you're active.
With Coronary Artery Disease, the vessels supplying your heart become narrowed or blocked, reducing oxygen to your heart muscle. This commonly triggers fatigue and breathlessness during physical activity. Your risk climbs dramatically with age—from just 0.2 per 100,000 in people under 25 to a whopping 1,252 per 100,000 in those aged 75-84.
What Causes Extreme Fatigue and Shortness of Breath in Autoimmune & Hormonal Disorders
Autoimmune and hormonal disorders create fatigue and breathing difficulties through entirely different mechanisms than heart and lung diseases.
ME/CFS (Myalgic Encephalomyelitis/Chronic Fatigue Syndrome) features crushing fatigue that worsens after even minimal physical or mental effort—a phenomenon called post-exertional malaise (PEM). Exciting recent research suggests ME/CFS involves problems with how your body delivers blood to tissues during exertion. After activity, symptoms can flare for days, leaving you bedridden and struggling to recover.
Long COVID shares striking similarities with ME/CFS, affecting roughly 25% of COVID-19 patients. Dr. Anthony Fauci has suggested they may be the same condition or very closely related. Both appear to involve "preload insufficiency"—basically, your peripheral nervous system fails to properly return blood to your heart during exertion.
When your thyroid gland underperforms (hypothyroidism), your entire metabolism slows down. This leads to profound fatigue, weakness, and sometimes breathlessness. About 17% of women will develop thyroid issues by age 60, with hypothyroidism being a frequent culprit behind unexplained fatigue.
Adrenal Issues affect your production of cortisol and other essential hormones. When your adrenal glands falter, you experience fatigue, weakness, and sometimes breathing difficulties, particularly during stressful situations.
Anemia reduces your blood's oxygen-carrying capacity, commonly causing both fatigue and shortness of breath. Iron deficiency anemia is especially widespread, affecting more than 5.6% of Americans, particularly women of childbearing age.
As explained in The Surprising Link Between Low Blood Flow and Fatigue, circulation problems can significantly contribute to these symptoms. At Juvenon, we understand that healthy blood flow and cellular function form the foundation of energy production and overall vitality.
Recognizing the Most Common Medical Culprits
When you're struggling with extreme fatigue and shortness of breath, pinpointing the underlying cause can feel overwhelming. These symptoms can arise from a surprisingly wide range of conditions—some temporary and others chronic.
Let's look at how acute and chronic causes differ:
| Acute Causes | Chronic Causes |
|---|---|
| COVID-19 | Asthma |
| Pneumonia | COPD |
| Pulmonary embolism | Heart failure |
| Heart attack | Anemia |
| Sudden blood loss | Hypothyroidism |
| Severe allergic reaction | ME/CFS |
| Carbon monoxide poisoning | Pulmonary hypertension |
| Upper airway obstruction | Obesity |
| Pneumothorax | Sleep apnea |
| Heart arrhythmia | Deconditioning |
Your lungs and heart are often the first places doctors look when these symptoms appear together. About 30 million Americans—that's over 11% of us—live with chronic lung disease, which restricts oxygen exchange and makes breathing require more effort. This extra work depletes your energy reserves, leading to that bone-deep fatigue.
Heart disease affects roughly 22 million Americans, and when your heart struggles to pump efficiently, your tissues don't receive the oxygen they need. The result? You feel both winded and exhausted, especially during activities that never bothered you before.
Those persistent respiratory infections can really knock you down too. Whether it's pneumonia, bronchitis, or COVID-19, your body uses tremendous energy fighting the infection while your lungs work below capacity. With COVID-19 specifically, about one in four patients develop lingering symptoms that can last months—a frustrating reality for many.
If you're feeling especially drained, anemia might be the culprit. This common blood condition affects more than 5.6% of Americans and means you have fewer red blood cells or less hemoglobin to transport oxygen throughout your body. No wonder you're tired and breathless!
Thyroid problems often fly under the radar, especially in women. About 17% of women will develop a thyroid disorder by age 60. When your thyroid is underactive (hypothyroidism), your metabolism slows down, causing fatigue that sleep doesn't fix. In severe cases, it can even affect your breathing.
And let's talk about sleep apnea—more than a third of U.S. adults snore at least a few nights weekly, and many have undiagnosed sleep apnea. Those breathing interruptions during sleep prevent restful sleep, leaving you exhausted during the day, regardless of how many hours you spent in bed.
For cancer patients, fatigue is almost universal—up to 90% of those receiving radiation therapy and 80% undergoing chemotherapy report significant fatigue. These treatments can affect lung function and how your body uses oxygen, contributing to both exhaustion and breathlessness.
Cardiac & Pulmonary Drivers
The heart and lungs work as inseparable partners in delivering oxygen and removing carbon dioxide. When one falters, the other often struggles too.

Heart rhythm problems (arrhythmias) can significantly reduce how much blood your heart pumps with each beat. Some arrhythmias announce themselves with palpitations and breathlessness, while others might primarily show up as unexplained fatigue that doesn't improve with rest.
If you have heart valve problems, they can either restrict blood flow or allow blood to leak backward, forcing your heart to work harder. Over time, this extra workload leads to fatigue, while the reduced forward flow causes shortness of breath, especially when you're active.
Interstitial lung disease is particularly sneaky. This group of disorders causes scarring of lung tissue, making it difficult for oxygen to pass into your bloodstream. The resulting low oxygen levels cause fatigue, while the stiff lungs make breathing difficult—a double whammy that can severely impact quality of life.
When fluid accumulates around your lungs (pleural effusion), it restricts their ability to expand fully. This not only makes you short of breath but also triggers your body's stress response. Combined with reduced oxygen levels, this chronic stress leaves you feeling utterly drained.
According to research on shortness of breath causes, most cases of dyspnea stem from heart or lung conditions, though many other factors can contribute.
Sometimes standard tests like chest X-rays, echocardiograms, and lung function tests don't reveal the cause. In these cases, your doctor might recommend cardiopulmonary exercise testing (CPET). This advanced test measures how well your heart and lungs work together during physical activity, often uncovering conditions that resting tests miss.
Systemic, Infectious & Treatment-Related Factors
Beyond heart and lung conditions, several systemic factors can leave you feeling both breathless and exhausted.
The flu and pneumonia temporarily impair lung function while simultaneously draining your energy as your immune system battles the infection. This combination commonly causes both fatigue and breathlessness that improve as you recover.
COVID-19 deserves special attention because of its significant impact. About 25% of COVID patients develop post-acute syndrome, with persistent fatigue and breathlessness that can last weeks or months after the initial infection resolves. Many people describe this as feeling like they're "running on half a tank" even months later.
Cancer treatments can cause profound fatigue through multiple mechanisms. Between anemia, muscle weakness, and direct cellular damage, it's no wonder that up to 90% of radiation therapy patients and 80% of chemotherapy patients report significant fatigue that affects their daily activities.
Many common medications can cause fatigue or breathing difficulties as side effects. Beta-blockers can cause fatigue and limit exercise capacity. Opioids can suppress your respiratory drive. Common antihistamines often cause drowsiness that feels like fatigue. Some antidepressants and antipsychotics cause fatigue, and diuretics can lead to electrolyte imbalances that cause weakness.
Beyond iron deficiency, other vitamin deficiencies can drain your energy too. Low levels of B12, folate, vitamin D, and magnesium commonly cause fatigue. In severe cases, these deficiencies can even affect your respiratory muscle strength, making breathing more difficult.
As kidney function declines in chronic kidney disease, toxins accumulate, anemia develops, and fluid balance gets disrupted. These changes commonly cause fatigue, and fluid accumulation can lead to shortness of breath, especially when lying down.
For more information on how circulatory issues contribute to these symptoms, check out our article on Understanding Poor Blood Circulation: Symptoms, Causes, and Treatments.
Lifestyle and Mental Health Triggers You Shouldn't Ignore
Not all causes of extreme fatigue and shortness of breath stem from medical conditions. Sometimes, the culprits are hiding in plain sight—in our daily habits and mental health.

Your body whispers before it screams. That persistent tiredness and trouble catching your breath might actually be your body's response to how you're living day to day.
Stress and burnout have become unwelcome companions in our world. When you're constantly in "fight-or-flight" mode, your body produces stress hormones that, over time, can leave you completely drained. You might notice yourself taking quick, shallow breaths during stressful moments—this can actually mimic the sensation of breathlessness. As one client told me, "I thought I had a lung problem, but my doctor said I was just breathing from my chest all day due to work stress."
Sleep—or lack thereof—plays a crucial role too. Poor sleep quality affects more than one-third of adults, who simply aren't getting the recommended 6-9 hours of restful sleep. Without proper rest, your body can't recharge, leading to that dragging fatigue that coffee just can't fix. Plus, sleep deprivation can make breathing difficulties feel much worse than they actually are.
Have you been less active lately? Deconditioning happens faster than most people realize. Just a few weeks of reduced physical activity can weaken your heart and respiratory muscles. This creates a frustrating cycle—you feel too tired to exercise, which makes you more deconditioned, which makes you even more tired and breathless with minimal effort.
Your eating habits matter tremendously. Overeating requires your body to divert extra energy to digestion, and the potential weight gain increases the work of breathing. On the flip side, undereating deprives your cells of the nutrients they need to generate energy. Both can leave you exhausted and breathless.
That glass of wine to help you unwind? Excessive alcohol might help you fall asleep initially, but it disrupts your deep sleep cycles, leading to poor-quality rest and daytime fatigue. Alcohol can also suppress your respiratory drive, especially in larger amounts.
The mind-body connection is powerful. Anxiety and depression frequently cause both fatigue and breathing changes. With anxiety, you might experience that "can't catch my breath" feeling during moments of worry. Depression often brings a bone-deep fatigue that makes even simple tasks feel overwhelming, and can subtly alter your breathing patterns.
According to research on work stress and burnout, the chronic workplace pressure many of us face can manifest as physical symptoms including both fatigue and breathing difficulties. The silver lining? Lifestyle changes can make a remarkable difference.
Simple Habits to Reduce Everyday Fatigue & Breathlessness
The good news is that small, consistent changes can help restore your energy and ease breathing difficulties when lifestyle factors are at play.
Your bedroom should be a sanctuary for sleep. Practice good sleep hygiene by sticking to consistent sleep and wake times—yes, even on weekends. Create a wind-down routine that avoids screens, caffeine, alcohol, and heavy meals in the hours before bedtime. Make your sleep environment cool, dark, and quiet. These simple changes can dramatically improve sleep quality.
What you eat directly impacts your energy levels. A balanced diet rich in iron, B vitamins, and antioxidants provides the building blocks your body needs for energy production. Many of my clients find that eating smaller, more frequent meals prevents energy crashes and reduces the breathing effort required after large meals.
Movement is medicine—but start where you are. If you've been inactive, moderate exercise beginning with just 10 minutes of walking daily can improve your cardiovascular fitness over time. Listen to your body and gradually increase duration and intensity as you get stronger. One client told me, "I could barely walk to my mailbox without getting winded. Now I'm doing 20-minute walks around the neighborhood."
Your breathing pattern itself matters. Breathing exercises like diaphragmatic breathing (belly breathing) and pursed-lip breathing can strengthen respiratory muscles and improve oxygen exchange. Practice these techniques for 5-10 minutes several times daily—they're especially helpful during moments of stress or exertion.
Learn to work with your energy, not against it. Pacing and rest involve breaking activities into smaller segments with rest periods in between. This energy conservation technique is particularly valuable if you're dealing with ME/CFS, long COVID, or cardiopulmonary conditions. As one client with long COVID shared, "I learned to fold laundry in three sessions instead of pushing through and then being bedridden for days."
For more strategies to combat mental fatigue specifically, our article on 7 Tips to Restore Mental Energy offers practical guidance.
At Juvenon, we understand that your energy begins at the cellular level. Our scientifically formulated supplements support mitochondrial function—your cells' energy factories—to help maintain natural vitality and stamina throughout your day.
Getting the Right Diagnosis—and When to Seek Help
When you're battling extreme fatigue and shortness of breath, knowing when to reach out for medical help can feel overwhelming. Let's walk through this together – finding answers starts with knowing what steps to take.
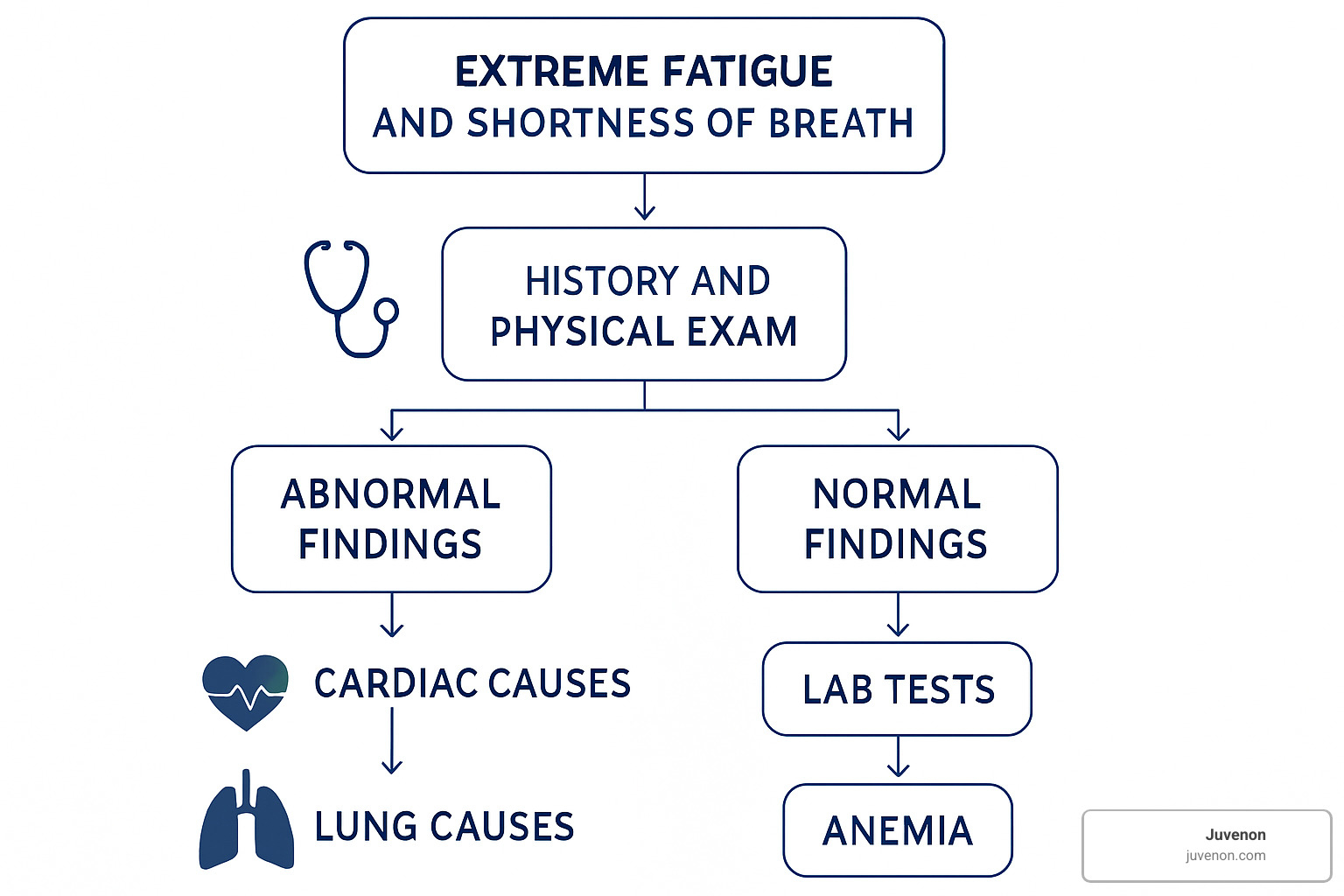
Here's a visual guide to help you understand what typically happens when you seek help:
Your body often sends clear warning signals when something serious is happening. Red-flag symptoms that shouldn't be ignored include sudden, severe breathing difficulties that feel different than usual exertion. Chest pain or pressure – especially if it radiates to your jaw or arm – needs immediate attention. If you've experienced fainting or severe dizziness, that's your body urgently trying to tell you something's wrong.
Other warning signs include blue discoloration of your lips or skin (called cyanosis), high fever coupled with breathing problems, unexpected swelling in your feet or ankles, or wheezing (that high-pitched sound when breathing).
When should you actually make that call? Here's a simple timeline:
For those red-flag symptoms I just mentioned, don't wait – call 911 immediately. Your body needs help now. For new breathlessness that's concerning but not severe, try to see a doctor within 24-48 hours. And for that dragging fatigue that just won't let up after 2-3 weeks? Schedule a regular appointment to get to the bottom of it.
When you do see your doctor, expect a conversation about your symptoms and medical history. They'll perform a physical exam focusing on your heart and lungs, and likely order some basic tests. Depending on what they find, you might be referred to specialists who can dig deeper into specific concerns.
These symptoms can stem from countless causes – finding yours might take some detective work and patience.
Key Tests Doctors Use
Diagnosing what causes extreme fatigue and shortness of breath usually involves several important tests to uncover the underlying issue.
Your doctor will likely start with a CBC (Complete Blood Count) – this simple blood test checks for anemia, infection, and inflammation. Did you know anemia affects more than 5.6% of Americans? It's a surprisingly common cause of both fatigue and breathlessness.
A thyroid panel measures those crucial hormones that regulate your metabolism. This is particularly important for women, as about 17% will develop a thyroid disorder by age 60. Your doctor might also check your ferritin levels to measure your iron stores, which can be low even when other blood tests look normal.
For heart-related concerns, a BNP test (B-type Natriuretic Peptide) helps identify if heart failure might be causing your symptoms. If sleep issues are suspected, a sleep study can diagnose conditions like sleep apnea – which affects many more people than you might think. More than one-third of American adults snore regularly, and many have undiagnosed sleep disorders.
An echocardiogram uses ultrasound to create pictures of your heart, showing how well it's pumping (normally at 50-70% efficiency). For particularly puzzling cases, your doctor might recommend an invasive CPET (Cardiopulmonary Exercise Testing), which measures how your heart and lungs function during physical activity – often revealing problems that don't show up when you're resting.

Sometimes symptoms persist despite normal initial testing. Don't get discouraged – this is when specialized evaluation becomes especially valuable. Advanced testing can help diagnose conditions like ME/CFS, pulmonary hypertension, or heart failure with preserved ejection fraction that might otherwise be missed.
When to Call 911
Some situations simply can't wait for a scheduled appointment. Trust your instincts, and call 911 immediately if you experience:
Chest pain that feels crushing or squeezing is never something to ignore. This sensation, especially when it radiates to your jaw or arm, could signal a heart attack. Bluish lips or skin (what doctors call cyanosis) means your body isn't getting enough oxygen – a serious emergency.
If you experience sudden severe breathlessness that comes on within minutes, particularly with a feeling of doom, don't wait to see if it improves. Similarly, fainting or near-fainting episodes combined with breathing difficulties need immediate attention.
Watch for rapid swelling of your face, throat, or tongue, which might indicate a severe allergic reaction that can quickly become life-threatening.
Heart attacks, pulmonary embolism (blood clot in the lungs), pneumothorax (collapsed lung), and severe asthma attacks are all medical emergencies where minutes truly matter. I know it can feel uncomfortable to "make a fuss," but please don't hesitate to seek emergency care when experiencing severe symptoms. Medical professionals would much rather check you and find nothing serious than have you wait until it's too late.
Managing & Treating the Underlying Cause
When it comes to tackling extreme fatigue and shortness of breath, treatment plans are as diverse as the conditions causing these symptoms. The right approach depends entirely on getting to the root of your specific issue.
For heart failure patients, treatment typically involves a combination of medications including ACE inhibitors to relax blood vessels, beta-blockers to reduce heart workload, and diuretics to decrease fluid buildup. Your doctor might recommend lifestyle changes like cutting back on salt and limiting fluids. In some cases, devices such as pacemakers or defibrillators may help. I've seen promising research on newer medications like SGLT2 inhibitors that show real potential for people with diastolic heart failure.
Those managing COPD often find relief through bronchodilators that open airways and combination medicines that pair these with steroids to reduce inflammation. Pulmonary rehabilitation programs can be life-changing, teaching breathing techniques and exercise strategies that make daily activities more manageable. For those with advanced disease, oxygen therapy or surgical options might be considered. Of course, if you smoke, quitting is absolutely essential to slow disease progression.
If anemia is behind your symptoms, treatment focuses on addressing what's causing your low red blood cells. This might mean taking iron supplements, vitamin B12, or folate, depending on your specific type of anemia. In severe cases, blood transfusions can provide immediate relief while you work on the underlying issue.
For people with hypothyroidism, thyroid hormone replacement therapy (typically levothyroxine) can restore normal metabolism and bring energy levels back to normal. Most patients notice improvements within weeks of starting treatment.
ME/CFS and Long COVID present unique challenges. While there's currently no cure for these conditions, management focuses on carefully pacing activities to prevent post-exertional malaise—that crash that comes after overexertion. Learning to work within your energy envelope becomes crucial. Research is ongoing, and I'm hopeful we'll see more treatment options in the coming years.
Sleep apnea treatment typically centers around CPAP therapy, which provides a steady stream of air pressure during sleep to keep airways open. Weight management and positional therapy (avoiding sleeping on your back) can also help in many cases.
For anxiety and depression, a combination of cognitive-behavioral therapy, medication, stress-reduction techniques, and lifestyle changes often yields the best results. These conditions can significantly drain your energy, but with proper treatment, many people see gradual improvement over several months.
If you're looking for natural approaches to boost your energy while addressing the underlying cause, check out our article on 5 Natural Energy Supplements to Fight Fatigue.
At Juvenon, we understand that cellular health—particularly mitochondrial function—is fundamental to energy production. Our scientifically formulated supplements support these processes naturally, helping your body produce energy at the cellular level.
Home Strategies to Boost Energy & Breathing
While you're working with your doctor on treating the underlying cause, these practical self-care strategies can help manage your symptoms day-to-day:
Diaphragmatic Breathing strengthens your primary breathing muscle and improves oxygen exchange. Think of it as physical therapy for your diaphragm:

To practice, lie on your back with your knees bent. Place one hand on your chest and the other on your abdomen. Breathe in slowly through your nose, focusing on making your abdomen rise while keeping your chest relatively still. Then exhale slowly through pursed lips. Just 5-10 minutes of practice several times daily can make a remarkable difference.
Pursed-Lip Breathing is particularly helpful during activities that leave you short of breath. Breathe in through your nose for a count of two, then purse your lips as if you're about to whistle and exhale slowly for a count of four. This technique helps keep airways open longer during exhalation and can provide immediate relief during moments of breathlessness.
Interval Activity is a game-changer for managing daily tasks. Rather than pushing through until exhaustion, break activities into smaller segments with built-in rest periods. Fold some laundry, then sit down for a few minutes before continuing. Prepare part of a meal, rest, then finish up. Using a wheeled cart instead of carrying items can also conserve precious energy.
Staying hydrated is crucial, as dehydration can worsen fatigue. Aim for 6-8 glasses of fluid daily unless your doctor has advised fluid restriction. I recommend keeping a water bottle nearby as a visual reminder to sip throughout the day.
Switching to small, frequent meals can help manage both fatigue and breathlessness. Large meals require significant energy for digestion and can actually increase breathlessness, especially if you have heart or lung conditions. Lighter, more frequent meals are often easier on your system.
While these strategies can significantly improve your quality of life, they should complement—not replace—professional medical care for serious underlying conditions.
Prognosis: What to Expect Long-Term
The long-term outlook for those experiencing extreme fatigue and shortness of breath varies considerably depending on what's causing these symptoms.
For those with heart and lung diseases, these conditions typically require lifelong management, but many people achieve good quality of life with proper treatment. Heart failure prognosis has improved dramatically with modern therapies, though the statistics remain sobering—up to half of patients may die within five years without treatment. This underscores the importance of early diagnosis and consistent management.
If anemia is your culprit, there's excellent news—once corrected, symptoms typically resolve completely. Depending on the cause, you might need ongoing monitoring to ensure the anemia doesn't return, but most people return to their normal energy levels.
Those with thyroid disorders usually see significant improvement within weeks to months of starting hormone replacement therapy. The key is finding the right dosage, which may require adjustments based on how you feel and your lab results.
ME/CFS and Long COVID often follow a more unpredictable course. Some patients improve significantly over time, while others experience persistent symptoms with periods of relative improvement and worsening. Learning to manage your energy through careful pacing becomes essential for quality of life.
People with sleep apnea frequently report dramatic improvement in energy levels once they start CPET therapy, sometimes within days of beginning treatment. The challenge is consistent use of the device, but those who stick with it often find it life-changing.
For anxiety and depression, energy levels typically improve gradually over weeks to months with appropriate treatment. The journey isn't always linear, but many people find their way back to feeling like themselves again.
Lifestyle-related causes often show the most dramatic improvement with appropriate changes. Deconditioning can reverse with gradual, consistent exercise, and stress-related fatigue typically improves with effective stress management techniques.
Regular follow-up care is essential for monitoring your progress and adjusting treatment as needed. Many conditions require periodic testing to ensure you're getting optimal management, and your treatment plan may evolve over time as new therapies become available or as your condition changes.
While managing chronic conditions can be challenging, many people find that with the right treatment approach, they can return to activities they enjoy and maintain a fulfilling quality of life.
Frequently Asked Questions about Extreme Fatigue and Shortness of Breath
Can anxiety really cause both fatigue and breathlessness?
Yes, anxiety can absolutely cause both extreme fatigue and shortness of breath. It's more common than many people realize.
When anxiety strikes, your breathing often shifts into a rapid, shallow pattern—what doctors call hyperventilation. This inefficient breathing makes you feel short of breath even though your oxygen levels are perfectly normal. It's like running your car engine in the wrong gear—you're working harder but getting less benefit.
Meanwhile, anxiety keeps your body stuck in "emergency mode," flooding your system with stress hormones like cortisol and adrenaline. While helpful for actual emergencies, this constant state of high alert is incredibly draining over time. Think of it as leaving all the lights and appliances running in your house 24/7—eventually, the power bill comes due in the form of exhaustion.
Many of my patients describe getting caught in a frustrating cycle: anxiety triggers breathing changes, which create more anxiety, which further affects breathing, and on it goes. Breaking this cycle usually means addressing both the mind and body aspects of anxiety through therapy, relaxation techniques, breathing exercises, and sometimes medication. The good news? As anxiety improves, both the fatigue and breathlessness typically fade away.
How are ME/CFS and long COVID connected to these symptoms?
ME/CFS (Myalgic Encephalomyelitis/Chronic Fatigue Syndrome) and long COVID share remarkably similar patterns, with extreme fatigue and shortness of breath featuring prominently in both conditions.
The defining characteristic of ME/CFS is something called post-exertional malaise (PEM)—a dramatic worsening of symptoms after even minimal activity. Many long COVID patients report this exact same phenomenon. You might feel relatively okay one day, take a short walk, and then be bedridden for days afterward.
Recent research points to several shared mechanisms between these conditions:
First, there appears to be a problem with how blood returns to the heart during physical activity (what researchers call "preload insufficiency"). Second, the autonomic nervous system—which controls automatic functions like heart rate and breathing—doesn't regulate properly. Third, the cellular "power plants" (mitochondria) don't produce energy efficiently. And finally, there's ongoing low-level inflammation throughout the body.
Dr. Anthony Fauci has noted that long COVID may be essentially the same condition as ME/CFS or at least closely related. With about 25% of COVID patients developing long-term symptoms, understanding these connections has become increasingly important.
For those affected, management focuses on carefully pacing activities to avoid triggering PEM, along with treating individual symptoms. While there's currently no cure for either condition, the surge in long COVID cases has dramatically increased research interest, offering hope for better treatments in the future.
Which over-the-counter remedies actually help?
When it comes to extreme fatigue and shortness of breath, there's no one-size-fits-all remedy—what helps depends entirely on what's causing your symptoms. That said, several evidence-based options might provide relief in specific situations.
If iron deficiency is behind your fatigue, iron supplements can make a remarkable difference. However, don't start taking iron without confirming you need it—excess iron can actually be harmful. Your doctor can check this with a simple blood test.
B vitamins, particularly B12 and folate, support your body's energy production and red blood cell formation. These might help if you're deficient, which is more common as we age or if you follow certain diets. Many of my older patients notice improved energy after addressing B12 deficiency.
Vitamin D deficiency is surprisingly common, especially in northern climates or if you don't get much sun exposure. Low levels can contribute to fatigue, and supplementation often helps restore normal energy.
CoQ10 is a naturally occurring enzyme that supports cellular energy production. It may be particularly helpful if you're taking statin medications for cholesterol, as these can deplete your body's CoQ10 levels.
Magnesium deficiency can cause both fatigue and muscle weakness. If tests confirm you're low, supplementation may help restore your energy levels.
For breathing difficulties specifically, fewer over-the-counter options directly help, though saline nasal sprays can relieve congestion that affects breathing, and honey can soothe throat irritation.
At Juvenon, we focus on supporting your body's natural energy production at the cellular level. Our scientifically formulated supplements target mitochondrial function—the true source of your body's energy—rather than providing temporary stimulant effects.
Always check with your healthcare provider before starting any supplement regimen, especially when experiencing significant symptoms that might indicate a serious underlying condition requiring medical treatment.
Conclusion
When you're struggling with extreme fatigue and shortness of breath, finding answers can feel overwhelming. Throughout this guide, we've explored the many possible causes—from serious medical conditions to everyday lifestyle factors—that might be behind your symptoms.
These two symptoms often show up together for a good reason. They're both tied to how well your body delivers and uses oxygen—the essential ingredient your cells need to create energy. When this system breaks down anywhere along the way, you feel it as both tiredness and breathing difficulties.
Your heart and lungs are the usual suspects when these symptoms appear, but don't dismiss other possibilities. Conditions like anemia can leave you breathless and exhausted even when your heart and lungs are working perfectly. Thyroid problems can slow your entire metabolism, while post-viral syndromes like long COVID can trigger persistent fatigue that doesn't improve with rest.
I've seen many patients whose symptoms stemmed primarily from their daily habits. Chronic stress, poor sleep quality, being out of shape, or not eating well can drain your energy and affect your breathing more than you might expect. The good news? These are often the most fixable causes.
Getting to the bottom of your symptoms usually takes a step-by-step approach with your healthcare provider. Sometimes standard tests reveal the answer quickly, while other times more specialized testing like cardiopulmonary exercise testing becomes necessary to uncover what's happening during activity.
Remember—treatment always needs to target the root cause. While breathing exercises and energy conservation techniques can help you feel better day-to-day, they're usually just part of the solution. And please, don't hesitate to call 911 if you experience severe symptoms like chest pain, blue lips, or fainting alongside your breathing troubles.
Here at Juvenon, we focus on supporting your body at the cellular level. Our supplements are designed to nurture your mitochondria—those tiny powerhouses inside your cells that convert nutrients into energy. While these formulations can support your natural vitality, they complement rather than replace medical care for serious symptoms.
If extreme fatigue and shortness of breath are affecting your quality of life, please reach out to a healthcare provider. With the right diagnosis and treatment plan, many people find significant relief and return to activities they love.
For more insights on improving circulation—a key factor in oxygen delivery and energy production—check out our article on blood-flow health.
Your journey back to feeling energetic and breathing comfortably might take time, but with proper care and patience, better days are ahead.























