
How to decrease blood sugar effectively comes down to a combination of diet, exercise, and lifestyle changes. If you're looking for immediate steps to lower your blood sugar levels, here are the most effective methods:
- Monitor your blood sugar regularly to understand your patterns
- Reduce carbohydrate intake, especially refined carbs and sugars
- Increase fiber consumption (25g for women, 35g for men daily)
- Stay hydrated with water instead of sugary beverages
- Exercise regularly (150 minutes of moderate activity weekly)
- Manage stress through meditation, yoga, or other relaxation techniques
- Get adequate sleep (7-8 hours nightly)
- Maintain a healthy weight (even 5% weight loss improves blood sugar)
High blood sugar, or hyperglycemia, affects millions of Americans. According to the CDC, over 34 million American adults have diabetes, and a staggering 1 in 3 adults have pre-diabetes – most of whom don't even know it. Left unchecked, liftd blood sugar can damage vital organs and lead to serious health complications.
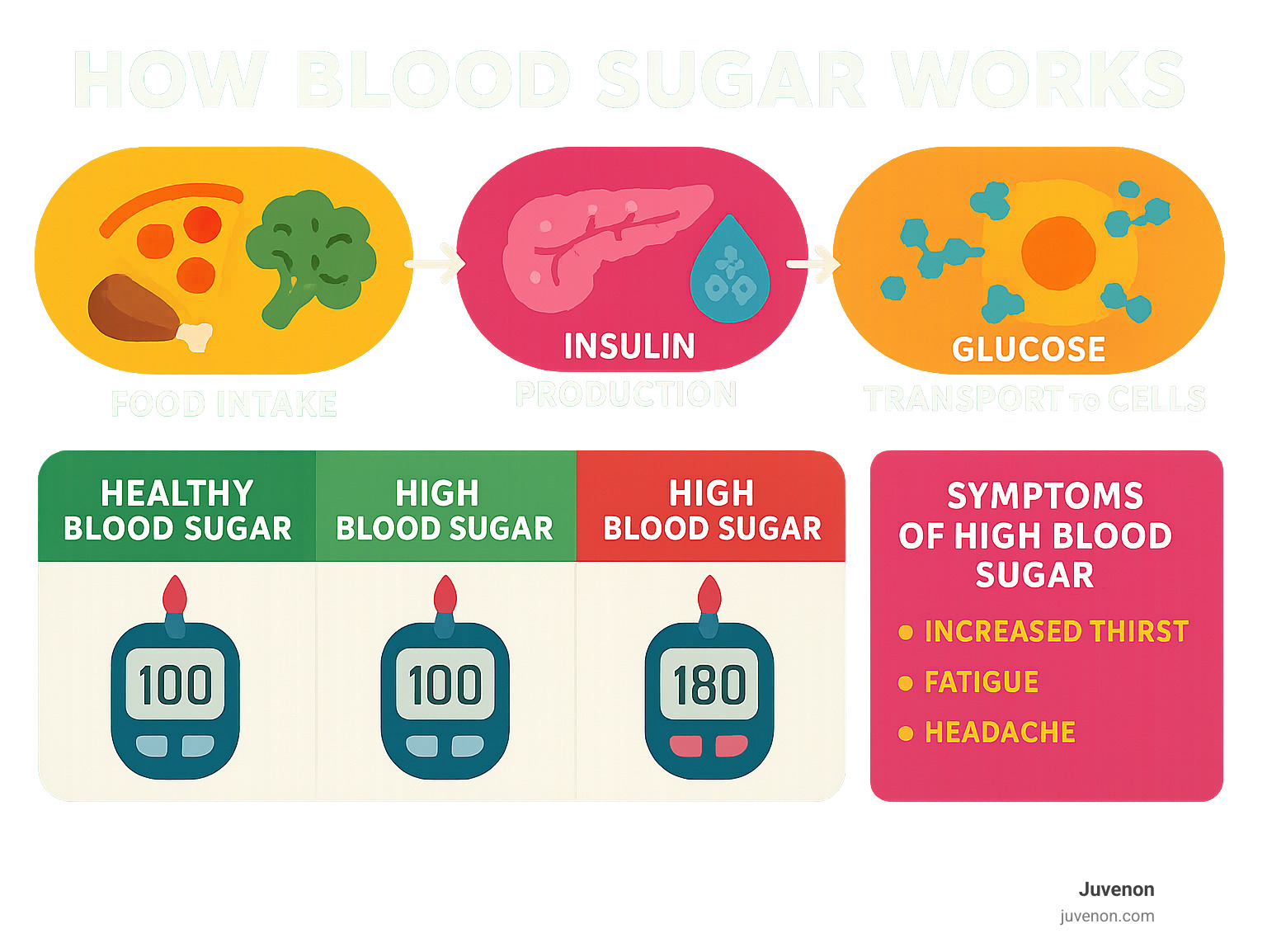
When your body can't properly use insulin to move glucose from your bloodstream into your cells, blood sugar levels rise. This happens either because your pancreas doesn't produce enough insulin (Type 1 diabetes) or because your cells have become resistant to insulin's effects (Type 2 diabetes).
I'm Michelle M. Henson, and as Head of Copywriting for Juvenon, I've spent years researching and writing about how to decrease blood sugar through evidence-based approaches that support healthy aging and metabolic function.
Blood Sugar Basics & Why It Matters
Think of glucose as your body's favorite fuel. When you enjoy a meal with carbohydrates, your digestive system breaks them down into glucose, which enters your bloodstream like tiny energy packets. Your pancreas then springs into action, releasing insulin – the helpful hormone that acts like a doorman, ushering glucose into your cells where it powers everything from your morning thoughts to your evening workout.
When this beautiful dance works as intended, your blood sugar levels stay within a healthy range. But for millions of Americans – including the 34 million with diabetes and the one-in-three adults with prediabetes – this system gets disrupted. Either the pancreas can't produce enough insulin (Type 1 diabetes) or your cells start ignoring insulin's signals (Type 2 diabetes).
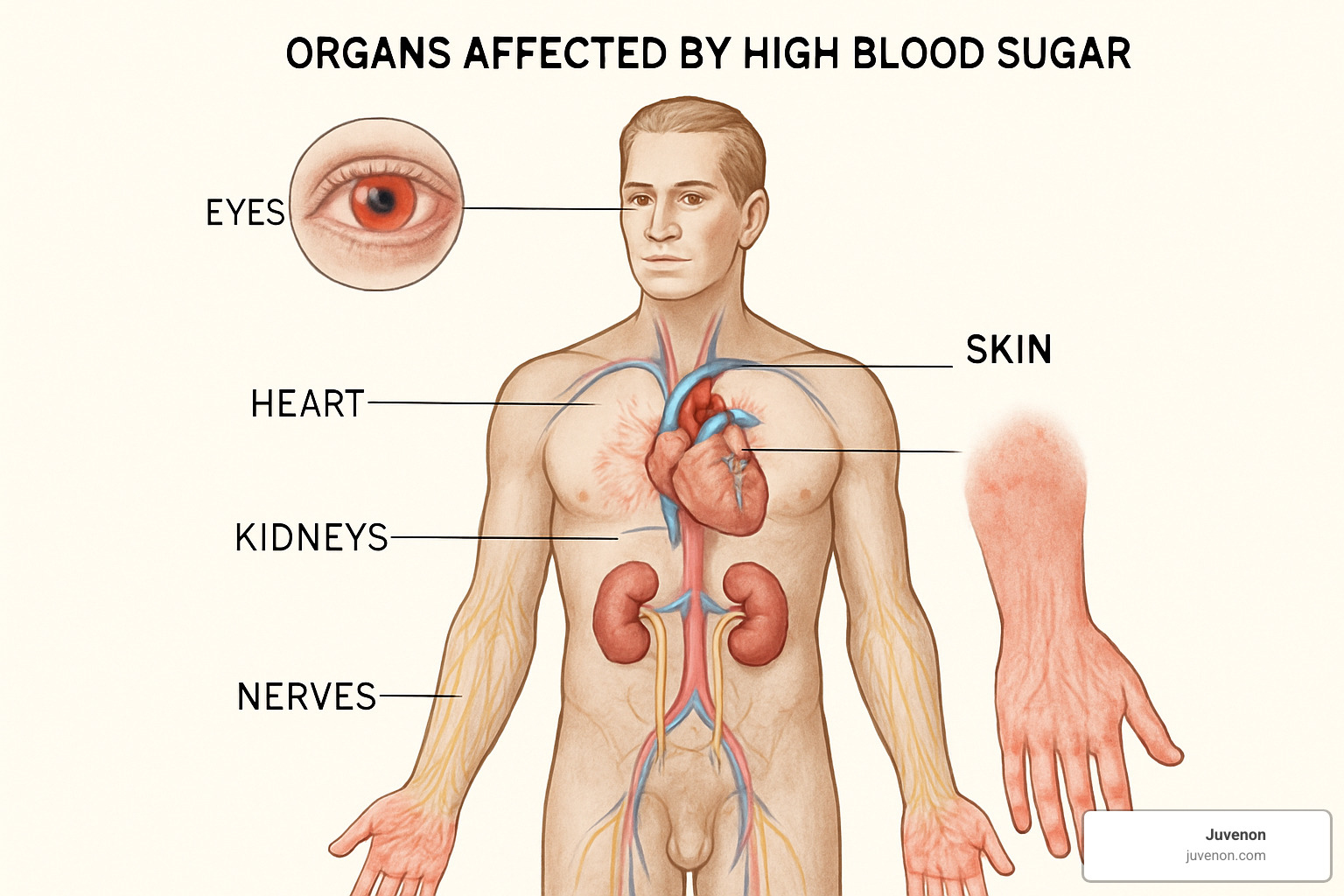
The result? Glucose gets stranded in your bloodstream instead of fueling your cells, and over time, this excess sugar can damage blood vessels and nerves throughout your body. It's like having too much traffic on your body's highways – eventually, things start breaking down.
These high blood sugar levels can affect virtually every part of your body:
- Heart and blood vessels: Your risk of heart attack, stroke, and peripheral artery disease climbs
- Kidneys: These amazing filters can become damaged or even fail
- Eyes: The delicate blood vessels in your retina may leak, potentially leading to vision loss
- Nerves: Damage causes that tingling, numbness, or pain (neuropathy) you might feel in your feet or hands
- Skin: Wounds heal more slowly, and infections become more likely
You might also experience the "dawn phenomenon" – a natural but frustrating morning rise in blood sugar caused by hormonal changes while you sleep. For people with diabetes, this can make mornings particularly challenging.
In severe cases, very high blood sugar can trigger diabetic ketoacidosis – a serious condition that announces itself with the "3 P's": polydipsia (excessive thirst), polyuria (frequent bathroom trips), and polyphagia (unusual hunger). If you notice these symptoms along with fruity-smelling breath, nausea, or confusion, seek medical help immediately.
Target Numbers at a Glance
Knowing your target range is like having a roadmap for how to decrease blood sugar effectively. While your healthcare provider might set personalized goals, here are the general guidelines:
Fasting blood glucose: 80-130 mg/dL before meals Post-meal (1-2 hours after eating): Less than 180 mg/dL
Danger zone: Above 240 mg/dL (check for ketones) Emergency: Above 300 mg/dL (especially with symptoms)
If your readings exceed 240 mg/dL, it's crucial to check your urine for ketones. The presence of ketones alongside high blood sugar can signal diabetic ketoacidosis, requiring immediate medical attention.
Your age, overall health, and other factors might influence these targets, so always work with your healthcare team to establish your personal goals. For deeper insights into hyperglycemia and its effects, the scientific research on hyperglycemia offers valuable information backed by medical experts.
How to Decrease Blood Sugar: 14 Evidence-Backed Steps
Ready to take control of your blood sugar? Let's explore practical, science-backed strategies that can make a real difference in your glucose management journey. I've gathered these approaches from the latest research and expert recommendations to help you create a sustainable plan that works for your lifestyle.
Step 1 – Track & Learn Your Numbers: First Move to Know How to Decrease Blood Sugar
Before making changes, you need to understand your starting point. Think of blood sugar monitoring as your personal roadmap—it shows where you are and helps you see if you're heading in the right direction.
Most people find that using a simple glucometer works well for regular testing. If you're looking for more detailed insights, continuous glucose monitors (CGMs) offer real-time tracking that can reveal how your body responds to different foods and activities throughout the day.
One technique I love recommending is paired testing—checking before a meal and again 1-2 hours after eating. This simple practice can be eye-opening! You might find that your "healthy" breakfast cereal sends your numbers soaring while a protein-rich alternative keeps them steady.
"Knowing your numbers is empowering," says Dr. Sarah Johnson, endocrinologist and Juvenon scientific advisor. "It takes the guesswork out of diabetes management and helps you make informed decisions."
Many smartphone apps now make tracking painless—some even create graphs that help spot patterns. These digital tools are especially helpful when sharing information with your healthcare team during appointments.
Step 2 – Smart Carb Choices & the GI: Cornerstone of How to Decrease Blood Sugar
Not all carbs are created equal—some are fast-burning fuels that send blood sugar soaring, while others provide steady, sustained energy. The glycemic index (GI) helps us understand this difference.
Think of low-GI foods (55 or lower) as slow-burning logs on a fire: whole grains like steel-cut oats and quinoa, colorful berries, crisp apples, hearty lentils, and vibrant vegetables. These foods release glucose gradually, helping you avoid those energy-draining spikes and crashes.
High-GI foods (70 or higher) are more like kindling—they create a quick flame that burns out fast. White bread, processed cereals, white rice, and sweetened drinks fall into this category. While they have their place, limiting these options helps keep your blood sugar more stable.
A simple swap can make a surprising difference. Replacing white rice (GI 73) with bulgur wheat (GI 48) can reduce post-meal blood sugar spikes by up to 33%—that's significant! For even better results, pair your carbs with protein or healthy fats. That apple with almond butter isn't just delicious—it's also a blood sugar-friendly snack.
Step 3 – Fiber & Portion Power
Fiber is your blood sugar's best friend. It slows down digestion, preventing those sharp glucose spikes that can leave you feeling drained hours later.
Women should aim for about 25 grams daily, while men need around 35 grams (or roughly 14 grams per 1,000 calories consumed). Soluble fiber deserves special attention—found in oats, beans, apples, and Brussels sprouts, it forms a gel-like substance in your digestive tract that specifically helps moderate blood sugar response.
The American Diabetes Association recommends a wonderfully simple approach to portion control: fill half your plate with non-starchy vegetables, a quarter with lean protein, and a quarter with healthy carbohydrates. This visual method makes healthy eating intuitive—no measuring cups or food scales required!
When snack cravings hit, reach for fiber-rich options that satisfy without spiking your glucose. A handful of mixed nuts, apple slices with almond butter, berries with Greek yogurt, or hummus with crisp vegetables all make perfect choices. As nutritionist Lisa Chen explains, "Fiber is nature's blood sugar stabilizer. It's like a sponge that slows the absorption of sugar into your bloodstream."
Step 4 – Hydration & Zero-Calorie Drinks
Something as simple as drinking enough water can make a meaningful difference in your blood sugar management. When you're dehydrated, your blood becomes more concentrated, which can lead to higher glucose readings.
Research consistently shows that well-hydrated people tend to have better blood sugar control. This makes perfect sense—your kidneys need plenty of fluid to efficiently filter excess glucose through urine.

Aim for at least 8 cups (64 ounces) of water daily, and more when it's hot or you're active. While plain water is ideal, unsweetened tea and zero-calorie beverages can also contribute to your daily intake. Just be sure to skip the sugary drinks, which can cause dramatic blood sugar spikes.
"Think of water as your body's natural detox system," says hydration specialist Dr. Mark Williams. "It helps flush excess glucose through your kidneys and keeps your blood flowing efficiently."
If plain water feels boring, try infusing it with refreshing cucumber slices, zesty lemon, or sweet berries. These natural flavor improvers make staying hydrated a pleasure rather than a chore.
Step 5 – Move More, Sit Less
Exercise might be the closest thing we have to a miracle drug for blood sugar management. When you're active, your muscles become more efficient at taking up glucose from your bloodstream—both during your workout and for hours afterward.
The sweet spot for most people is about 150 minutes of moderate activity each week. This could be brisk walking, swimming, cycling, or dancing—whatever gets your heart pumping and brings you joy. Adding resistance training twice weekly builds muscle mass, which acts as a glucose reservoir, helping regulate your blood sugar even when you're resting.
One of my favorite recommendations is incorporating "exercise snacks" throughout your day—short bursts of movement every 30 minutes or so. Even a 10-minute walk after meals can significantly reduce post-meal glucose spikes. Your active muscles literally pull sugar from your bloodstream to fuel your movement, no insulin required!
If your blood sugar reads above 240 mg/dL, check for ketones before exercising. If ketones are present, it's best to wait until levels normalize, as activity could temporarily raise your blood sugar further.
Step 6 – Shed 5% Body Weight
Here's an encouraging fact: you don't need dramatic weight loss to improve blood sugar control. Research shows that losing just 5% of your body weight can significantly improve insulin sensitivity and reduce medication needs for many people.
For someone weighing 200 pounds, that's just 10 pounds—a realistic and sustainable goal that can lead to meaningful health improvements. Rather than focusing on restrictive diets, consider gentle shifts like using smaller plates to naturally reduce portions, eating mindfully without distractions, and embracing the plate method we discussed earlier.
Many people find success with Mediterranean-style eating patterns, which emphasize vegetables, fruits, whole grains, olive oil, and lean proteins. This approach isn't just effective for weight management—it's also been shown to improve blood sugar control independently.
"Weight loss doesn't have to be dramatic to be beneficial," notes Dr. Elena Rodriguez, metabolic specialist. "Small, sustainable changes often yield the best long-term results for blood sugar management."
Step 7 – Manage Stress & Sleep
The mind-body connection plays a crucial role in blood sugar regulation. When stress levels rise, your body releases hormones like cortisol and adrenaline that can lift glucose levels—even if you haven't eaten a thing.
Similarly, poor sleep can trigger insulin resistance, making it harder for your cells to use glucose efficiently. This is why addressing these often-overlooked factors can make such a difference in your overall management plan.
For stress management, consider gentle practices like deep breathing exercises, meditation, yoga, or simply spending time in nature. These activities activate your parasympathetic nervous system—the "rest and digest" mode that counterbalances stress hormones.
Quality sleep deserves equal attention. Aim for 7-8 hours nightly, maintaining a consistent schedule even on weekends. Create a sleep sanctuary by keeping your bedroom cool, dark, and quiet. Limiting screen time before bed is especially important—the blue light emitted by phones and tablets can disrupt your natural sleep-wake cycle.
"Sleep is when your body resets its metabolic processes," explains sleep specialist Dr. James Chen. "Without adequate rest, insulin resistance increases, making blood sugar harder to control the next day."
Step 8 – Micronutrient & Gut Support
Certain nutrients and gut health strategies can provide additional support for how to decrease blood sugar naturally.
Chromium and magnesium both play important roles in glucose metabolism. You can boost your intake through foods like whole grains, broccoli, and nuts (rich in chromium) and leafy greens, seeds, and legumes (excellent sources of magnesium).
The connection between gut health and blood sugar control is a fascinating area of emerging research. Including probiotic-rich foods like yogurt with live cultures, tangy kefir, fermented vegetables, and tempeh may help improve insulin sensitivity by supporting a diverse and balanced gut microbiome.
Several supplements have shown promise in research studies. Apple cider vinegar (1-2 tablespoons diluted in water) may help reduce fasting blood sugar when taken regularly. Warming cinnamon (½ to 2 teaspoons daily) appears to improve insulin sensitivity. Berberine, a compound found in several plants, has demonstrated effects comparable to some diabetes medications in small clinical trials.
At Juvenon, we believe in evidence-based approaches to health and longevity. While our supplements are carefully formulated based on scientific research, we always recommend consulting your healthcare provider before starting any new supplement—especially if you have diabetes or take medications. Your safety and well-being are our top priorities.
When to Call Your Healthcare Team
Managing blood sugar is often a balancing act, and sometimes, despite your best efforts, you'll need professional medical support. Knowing when to reach out to your healthcare team is just as important as knowing how to decrease blood sugar on your own.
Trust your instincts if something feels off. Your body often sends signals when your blood sugar is dangerously high, and these aren't warnings to ignore.
If your blood sugar reading remains stubbornly above 300 mg/dL even after following your treatment plan, it's time to pick up the phone. This isn't something to "wait and see" about – persistent high readings can quickly lead to complications that are harder to address the longer you wait.
Another red flag is finding ketones in your urine when your blood sugar exceeds 240 mg/dL. This combination can signal the beginning of diabetic ketoacidosis, a serious condition that requires prompt medical attention. Most home glucose monitoring kits include ketone testing strips – they're worth keeping on hand if you have diabetes.

Pay attention to physical symptoms too. Blurred vision isn't just inconvenient – it can be your body's way of telling you that high blood sugar is affecting your eyes. Extreme fatigue that doesn't improve with rest or wounds that seem to heal at a snail's pace are also signs that your blood sugar might be undermining your health.
Don't hesitate to call your doctor if you have questions about adjusting medication or insulin doses. These aren't decisions to make on your own, and your healthcare provider would much rather help you make safe adjustments than treat complications later.
In emergency situations, quick action can save lives. If you or someone you care for experiences confusion, difficulty breathing, fruity-smelling breath, or vomiting alongside high blood sugar, don't wait – call 911 or head to the emergency room immediately. These symptoms can indicate advanced ketoacidosis, which requires urgent medical intervention.
Your healthcare team isn't just there for emergencies. Regular check-ups and open communication form the foundation of effective blood sugar management. Your doctor, diabetes educator, and other specialists are partners in your health journey – they want to help you succeed in keeping your blood sugar within target ranges.
Many people find that bringing their blood glucose logs to appointments helps their healthcare team spot patterns and make more effective treatment recommendations. Whether you use a paper journal or a smartphone app, this information can be invaluable for fine-tuning your management plan.
Frequently Asked Questions about How to Decrease Blood Sugar
What are the "3 P's" of high blood sugar?
If you've been researching diabetes or blood sugar issues, you've probably come across the famous "3 P's." These are the classic warning signs that your blood sugar has climbed too high:
The first "P" is polydipsia – that unquenchable thirst that has you drinking glass after glass of water. The second is polyuria – making those frequent trips to the bathroom as your kidneys work overtime to flush out excess glucose. And the third is polyphagia – feeling hungry all the time, even after eating a full meal.
It's like your body is sending you urgent text messages! When blood sugar rises, it pulls fluid from your tissues (hello, thirst), your kidneys try to filter out the excess glucose through urine (hello, bathroom breaks), and your cells are starving for energy even though there's plenty of glucose floating around (hello, hunger pangs).
If you're experiencing this trio of symptoms – especially alongside fatigue, blurry vision, or cuts that seem to take forever to heal – it's time to check in with your healthcare provider. Your body is trying to tell you something important.
Can I lower blood sugar quickly in an emergency?
When blood sugar climbs into dangerous territory (above 240 mg/dL), the fastest and safest response is rapid-acting insulin as prescribed by your doctor. This isn't the time for DIY approaches – follow your healthcare provider's specific instructions for correction doses. Remember to wait at least three hours between insulin doses to prevent dangerous overlapping effects.
For those less urgent situations when your numbers are just a bit too high:
Water is your friend – staying hydrated helps your kidneys flush out excess glucose. A short walk around the block can help too, but only if you don't have ketones present (check first!). And it might seem obvious, but avoid eating carbs until your levels come down.
Important safety note: If you're experiencing symptoms like fruity-smelling breath, nausea, vomiting, or confusion along with high blood sugar, don't try to handle it at home. These could be signs of diabetic ketoacidosis – a serious condition that requires immediate medical attention. Call 911 or head to the emergency room right away.
Do natural supplements really work?
When it comes to natural supplements for how to decrease blood sugar, the evidence is... complicated. Some show promise, while others fall short of their marketing claims.
Berberine stands out from the crowd with the strongest scientific backing. Some studies even suggest it might be comparable to the prescription medication metformin – pretty impressive for a plant compound! Cinnamon might help some people improve insulin sensitivity, though the effect is usually modest. Alpha-lipoic acid has shown potential for supporting insulin function, and fenugreek seeds (either soaked or in supplement form) might help lower fasting glucose levels.
At Juvenon, we believe in the power of science-backed natural approaches. But we also believe in being straightforward: supplements should complement, not replace, the foundations of good blood sugar management – healthy eating, regular exercise, and proper medical care.
If you're considering adding supplements to your routine, please take these three important steps:
- Have a conversation with your healthcare provider first
- Think of supplements as part of your overall strategy, not a magic solution
- "Natural" doesn't automatically mean risk-free – supplements can interact with medications and have their own side effects
The most effective approach to managing blood sugar will always be a comprehensive one that combines lifestyle changes, medical supervision, and potentially, carefully selected supplements based on your individual needs.
Conclusion
Let's be honest – tackling high blood sugar isn't about finding some magical quick fix. It's about building sustainable habits that support your body's natural ability to regulate glucose. The 14 evidence-backed steps we've explored give you practical ways to how to decrease blood sugar while improving your overall health.
I've found in my own life that small, consistent changes often create the most lasting impact. Adding a brief walk after dinner, choosing brown rice instead of white, or prioritizing those crucial 7-8 hours of sleep might seem like minor adjustments, but they compound over time into significant improvements in your glucose control.
At Juvenon, we're passionate about supporting your journey toward better metabolic health. Our team formulates supplements based on rigorous scientific research, designed to complement the lifestyle strategies we've discussed. These products provide additional support for cellular health and energy production – the foundation of healthy aging.
If you're feeling overwhelmed by blood sugar management, please remember you're not walking this path alone. Millions of Americans face similar challenges every day. With the right knowledge, support system, and tools at your disposal, you can take meaningful steps toward stable blood sugar levels that help you feel energized and vibrant.
Before making significant changes to your diet, exercise routine, or adding supplements, have a conversation with your healthcare provider – especially if you have diabetes or take medications that affect blood sugar. Your doctor remains your most important partner in this journey.
For more information about how Juvenon's specially formulated supplements can support your metabolic health, visit our website for essential health supplements or reach out to our customer service team with questions.
Here's to your health – and the small, powerful changes that add up to transformative results!
























